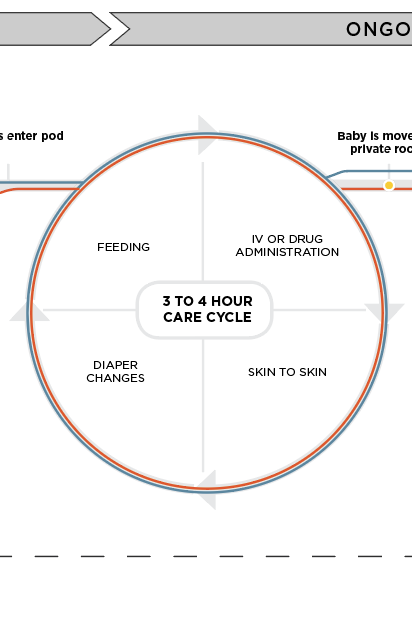
I visited 2 NICUs at separate instances with the intention of seeing firsthand how the NICU operates. I was able to have informal conversations with nurses and staff, and learned how the NICU operates on a relatively fixed routine.

Everything in the NICU operates on a routine after admission, with the care cycle taking place every 3 to 4 hours. After enough time, parents will acclimate and can begin to contribute to care responsibilities.





























.gif)
.gif)
.gif)
.gif)











.gif)